What are Micromanipulation Procedures?
New ART methods have been developed as a result of improvements in microscopic technology and our understanding of eggs, sperm, and embryos. Individual eggs, sperm, and embryos may undergo micromanipulation to increase the likelihood of pregnancy. These procedures call for specialized tools and personnel. Intracytoplasmic sperm injection (ICSI) is used to aid fertilization in cases of severe male factor infertility, assisted hatching, and aid embryo implantation. It is currently the most widely used micromanipulation technique. To maximize success, patients using these techniques should adhere to the specific instructions provided by their clinic.
Below are three of the most common micromanipulation procedures used in Assisted Reproductive Technology, namely, Intracytoplasmic Sperm Injection (ICSI), Assisted Hatching, and Embryo Biopsy
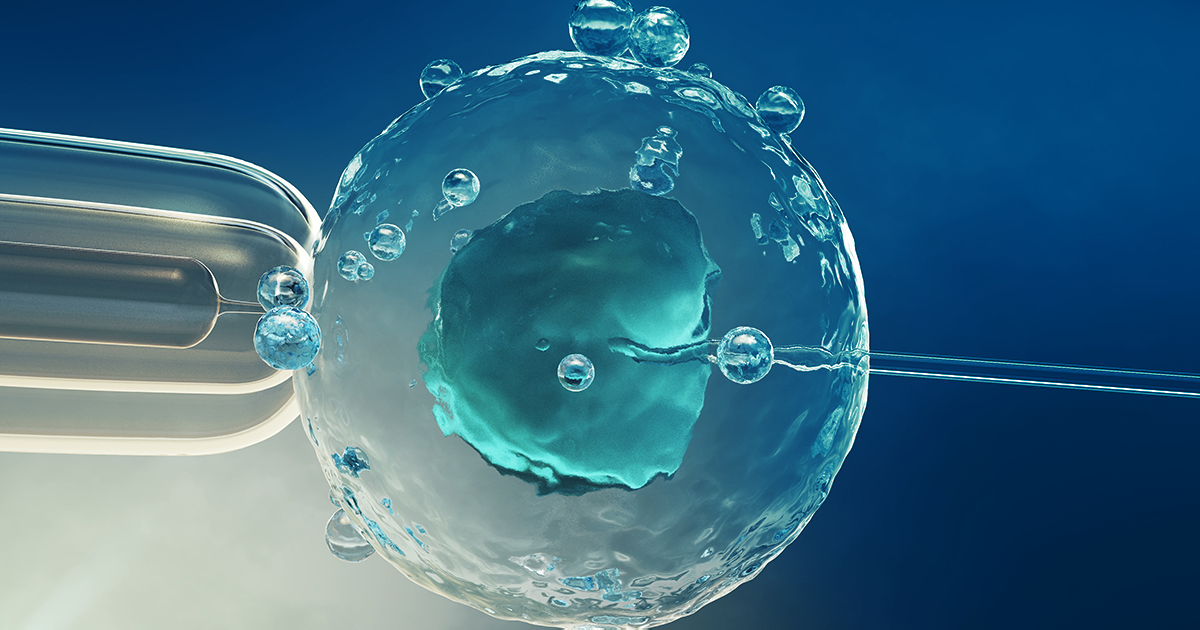
What is Intracytoplasmic Sperm Injection (ICSI)?
The goal of an Intracytoplasmic Sperm Injection (ICSI) procedure is to treat male factor infertility. These cases may include azoospermia, oligospermia, and asthenospermia which can be attributed to low sperm count, poor sperm motility, and abnormal sperm morphology, respectively.
The egg can be fertilized by injecting a single sperm into its cytoplasm. Combining enzyme treatment with microdissection allows for the release of mature eggs from their surrounding cells. The eggs are each individually injected with a single sperm using specialized micromanipulation apparatus. Injected eggs are placed back in the incubator in the lab and are cared for similarly to regular In Vitro Fertilization (IVF). Antisperm antibodies and sperm-attacking proteins that can be found in blood, seminal fluids, or vaginal fluids, can also be treated with ICSI.
The Pros and Cons of ICSI
ICSI has the advantage of making it possible to treat severe cases of male factor infertility that would not otherwise be treatable. IVF requires a minimum quantity of sperm that are normal in shape and motility. The chances of fertilization decrease dramatically when this minimum number of sperm is not available. In contrast, ICSI can theoretically be done with as few as a few sperm.
There are still a few treatments for severe male factor infertility besides ICSI. When couples with severe male factor infertility undergo traditional IVF, a donor sperm can increase the success rate of pregnancy. Through donor sperm, you can even cut back on costs and have a simpler treatment compared to IVF.
However, as with any medical treatment, ICSI still has some risks. The development of a genetically abnormal embryo is one of the possible outcomes of injecting a sperm that appears normal but is actually genetically abnormal. The majority of abnormal conceptions do not develop or implant in the uterus. ICSI appears to have a similar incidence of congenital abnormalities or birth defects to the general Assisted Reproductive Technology population. ICSI may increase the likelihood of sex chromosome abnormalities.
Nevertheless, research surrounding ICSI is still ongoing, and it is important to acknowledge that there are no known long-term risks associated with the procedure. Recent research indicates that some severe cases of male factor infertility may be genetic in nature and may be transmitted to male offspring via ICSI. Additionally, some kids in the general human population are born with congenital abnormalities that are not directly attributed to ICSI, and are generally out of a physician's control.
Despite the small risks, ICSI is the ultimate micromanipulation method as it manipulates both male and female gametes by directly inserting the sperm into the ooplasm to produce the best results.
Assisted Hatching
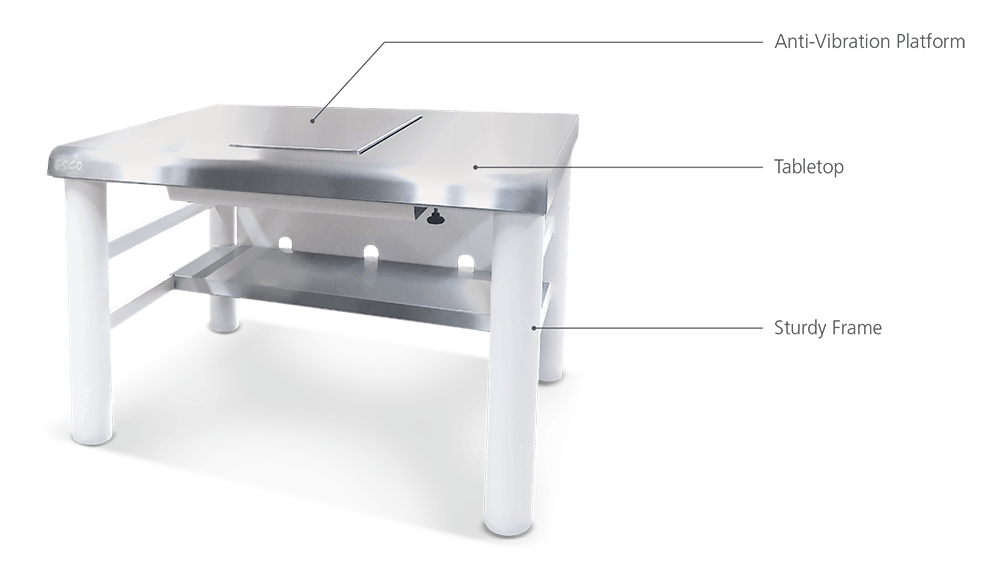
In Assisted Hatching, embryos are hatched at blastoctyst stage before transferred to the uterus. Day 5 embryos at blastocyst stage usually undergo the assisted hatching procedure. The blastocyst must hatch from the zona coating that originally encased the egg just prior to implantation. Just before the embryo transfer, a hole is made in the sac (zona pellucida) that surrounds the developing embryos to aid the hatching process. This entails either cutting the zona coating with a fine needle or laser or dissolving a portion of it with an acid solution. The procedure carries a small risk of harming the embryos and fragment removal. So this must be done under the microscope by trained personnel using specialized micromanipulation equipment such as Anti Vibration Tables (AVT).
Any modification to the zona pellucida's structure will hinder the hatching process because the embryo must exit it in order to undergo successful implantation. The embryo must have the ability to herniate and leave the zona pellucida on day 5 or 6 in order to prevent necrosis, regardless of whether the size and consistency of the outer shell are regular during in-vitro culture. The embryologist will perform assisted hatching by inserting a single artificial opening in the zona that was created either mechanically, chemically, enzymatically, or with laser assistance. This is done if a potential impairment of the hatching process is suspected.
Embryo Biopsy
The process of Embryo Biopsy starts with collecting the necessary genetic material for analysis. An Embryo Biopsy involves the embryologist removing a few cells from the embryo's outer layer, which will eventually become the placenta. The embryologist will remove cells from each embryo on day 5 to 7 of development, and sends the biopsy for genetic analysis. The laboratory examines the embryo to see if it has intact chromosomes. Geneticists will look for markers that indicate the presence of a specific heritable disease during the Preimplantation Genetic Diagnosis (PGD) analysis. Finally, the embryologist will arrange for embryo transfer and will only use unaffected embryos from the screening.
Preimplantation Genetic Diagnosis (PGD/PGS)
Physicians can help their patients give birth to healthy babies, thanks to technological advances that can identify chromosomally normal embryos and only transfer the healthy embryos to the uterus using Preimplantation Genetic Diagnosis/Screening or PGD/PGS.
Preimplantation Genetic Diagnosis or Screening (PGD/PGS) are techniques that can be used to check embryos for genetic disorders before they are transferred to the uterus. Couples or individuals with severe inherited disorders can use PGD and PGS to reduce the likelihood of passing on their condition to their potential offspring. These methods involve taking a cell out of an embryo using a micromanipulator. To ascertain whether the embryo is normal, this cell is sent to a diagnostic lab. The patient's chances of becoming pregnant with an affected child can be reduced by transferring acceptable embryos into her.
PGD/PGS has also been linked to an increase in pregnancies among some women who have chromosomal conditions that lower or increase miscarriage rates or embryo implantation rates.
Other Procedures used in ART
Apart from ICSI, Assisted Hatching, and embryo biopsy, there are other Micromanipulation Procedures used in Assisted Reproductive Technology (ART) as well.
Frozen Embryo Transfer
Embryo freezing is a crucial component of effective ART. The benefits of freezing are numerous, so embryologists recommend couples to have this choice. Without having to go through another ovarian stimulation and retrieval, these embryos offer a second or even third chance for pregnancy, because these can be used for subsequent attempts at pregnancy. Freezing the embryos can also increase the safety of an IVF cycle and help reduce the likelihood of multiple births by allowing for the transfer of fewer embryos during the fresh cycle.
Patients whose cycles have been coordinated with the stage of the frozen embryo can receive embryo transfers. As an alternative, embryos can also be moved throughout a natural cycle. Using liquid nitrogen, embryos can be kept indefinitely without losing viability.
Donor Eggs
As mentioned earlier, patients have the choice to look for donor eggs ART procedures as well. There are, however, a few factors to consider before choosing a donor egg to increase the chances of pregnancy. These factors include the matching of donor candidates and recipients, laboratory testing, genetic screening that is parallel to PGD/PGS, psychological tests, egg donor treatment, recipient treatment, and gestational carriers.