One of the most crucial developments in reproductive medicine is the introduction of assisted reproductive technology or ART. People can increase their chances of getting pregnant with procedures like intrauterine insemination (IUI) and in vitro fertilization (IVF). Additionally, patients have the option of using fresh or frozen sperm in these procedures.
Research presented at the annual meeting of the European Society of Human Reproduction and Embryology by Dr. Panagiotis Cherouveim of Massachusetts General Hospital and Harvard Medical School highlights that there is no significant difference in pregnancy rates between IUI cycles using fresh vs. frozen sperm.
The study looked at the results of more than 5000 IUI procedures. The overall pregnancy rates were not significantly different, but there were some variations between patients who underwent ovarian stimulation prior to insemination and those who did not. The majority of the frozen sperm used in this study, however, came from anonymous donors, who typically have better-quality sperm and are younger and healthier than the partners who provided fresh sperm samples. People are encouraged to keep this in mind as this is a limitation explicitly stated in the study.
Before we further examine the difference and success rates of fresh vs. frozen sperm, let's first discuss what IUI and IVF cycles are.
What are Intrauterine Insemination (IUI) Cycles?
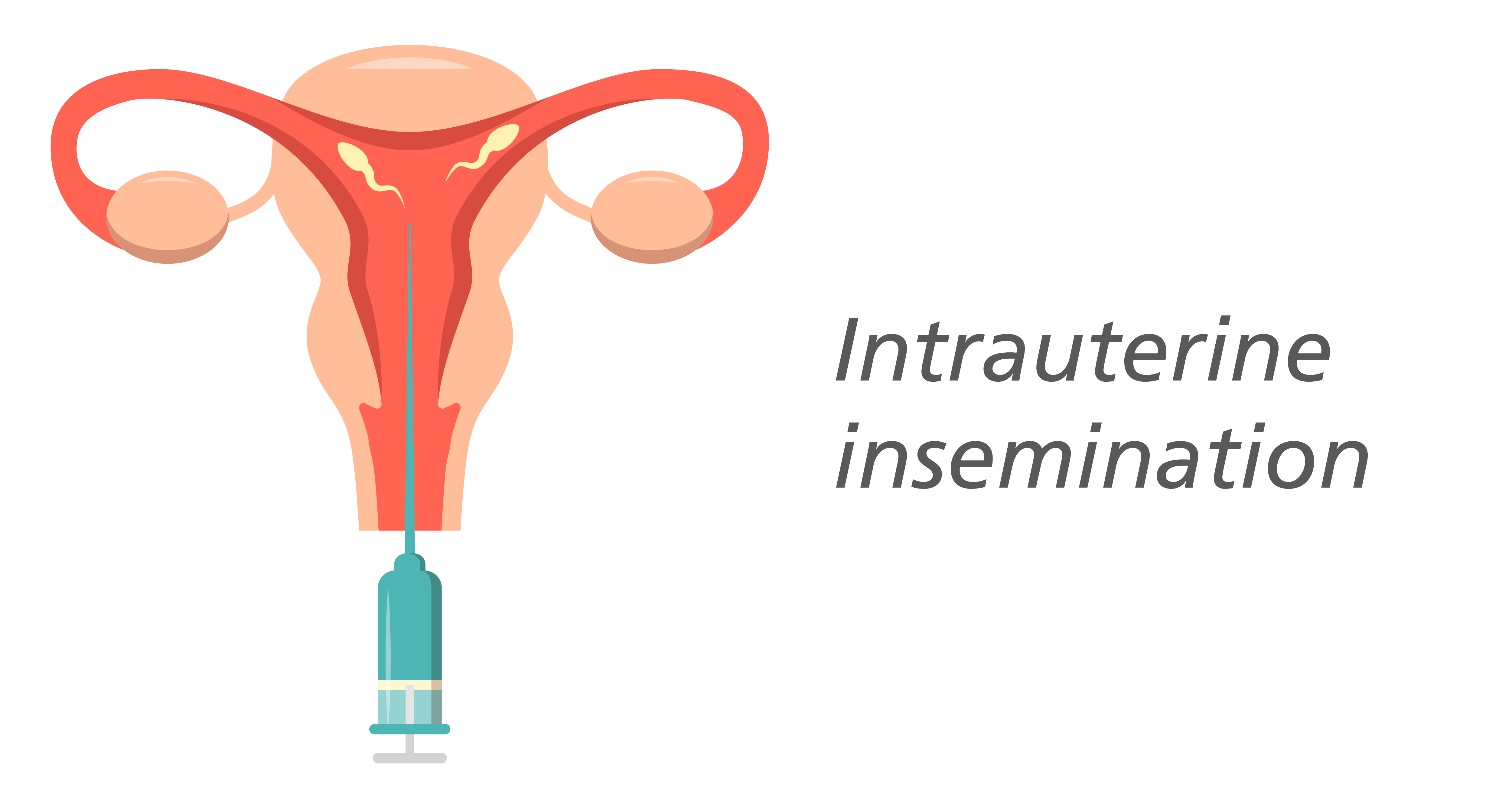
Intrauterine Insemination (IUI) Cycle is an artificial insemination technique that is commonly used to treat infertility. In an intrauterine insemination (IUI) procedure, concentrated and processed motile sperm are injected right into the uterus. Couples who are unable to reproduce through intercourse or who prefer to forego it sometimes use the low-cost, low-resource alternative of intravaginal insemination (IUI).
This process involves concentrated and washed sperm that are directly injected into the uterus once the ovary releases one or more eggs for fertilization. The intended result of intrauterine insemination is for the sperm to travel into the fallopian tube, fertilize an egg that is already mature, and develop into a pregnancy. Depending on the underlying causes of infertility, IUI can be timed to coincide with a patient's regular cycle or it can be done simultaneously with fertility medications.
The theory supporting the clinical application of IUI is that increasing the density of sperm high in the reproductive tract increases the likelihood of conception. Ovulation in the IUI cycle, the presence of at least one functional fallopian tube, the ability to successfully inseminate with a sufficient number of motile sperm, and the absence of any known or suspected active pelvic, intrauterine, or cervical infections are the minimum requirements for performing the procedure.
IUI is especially helpful in couples with certain types of severe sexual dysfunction (such as severe vaginismus, and ejaculatory dysfunction) or discordant for sexually transmitted disease carriage (like human immunodeficiency virus [HIV], hepatitis). IUI enables the sperm to avoid potentially dangerous cervical factors, increasing the number of sperm that reach the uterine cavity in cases of cervical factor or mild male factor infertility (and oocyte). Pregnancy rates are believed to be higher for women undergoing ovulation induction, including those with unexplained infertility or minimal or mild endometriosis, when IUI is used as an adjunctive procedure rather than timed natural intercourse. IUI is frequently used in these couples as a cost-effective, intermediate-level intervention before moving forward with in vitro fertilization (IVF).
IUI is also often the first choice for couples who stumble upon the struggles of infertility. In fewer cases, IUI is a good choice for endometriosis-related infertility, male infertility, cervical infertility, ovulatory infertility, and semen allergy.
The likelihood of getting pregnant after IUI is influenced by female, male, and technical factors which we will also discuss later in this article.
Risks of IUI Cycles
The risk of serious complications during intrauterine insemination is low and the procedure is generally simple and safe. There is a very small chance that the procedure will result in an infection. Sometimes a little vaginal bleeding can also occur as a result of inserting the catheter into the uterus. But usually, this has no impact on a woman's chance of getting pregnant. Finally, IUI by itself doesn't put women at an increased risk of having twins, triplets, or more pregnancies. However, there is a significant increase in the risk of multiple pregnancies when used in conjunction with ovulation-inducing drugs. Premature labor and low birth weight are two risks that are higher for multiple pregnancies than for single pregnancies.
What are In Vitro Fertilization (IVF) Cycles?

In vitro fertilization (IVF) involves a complex set of procedures, and is utilized to improve fertility, avoid genetic problems, and facilitate child conception. IVF is an assisted reproductive technology procedure that has had the most success. The couple's sperm and eggs are used in the procedure, making it possible. During IVF, eggs, sperm, or embryos from known or unidentified donors may also be used. An embryo that has been implanted in a woman's uterus may occasionally be used to carry the child.
IVF involves taking mature eggs out of the ovaries and fertilizing them with sperm in a lab. After that, the fertilized eggs are moved into a uterus. IVF cycles take about three weeks to complete. The process can occasionally take longer when these steps are broken down into separate steps.
Numerous factors, such as your age and the underlying cause of your infertility, can affect the success rates of IVF. Additionally, IVF can be pricy, invasive, and time-consuming. If more than one embryo is implanted during IVF, it may result in pregnancy with more than one fetus (multiple pregnancies).
Your physician and embryologist can explain the IVF's operation, potential risks, and suitability for you as a method of infertility treatment.
Infertility or genetic issues are treated with in vitro fertilization (IVF). Before attempting IVF, you and your partner may be able to try less invasive treatments such as fertility drugs to increase egg production or intrauterine insemination (IUI), in which sperm are directly injected into the uterus just before ovulation. Sometimes the first line of treatment for infertility in women over 40 is advised to be IVF. IVF may still be an option for you even if you have specific medical conditions.
Patients with fallopian tube damage or blockage, ovulation disorders, endometriosis, uterine fibroids, prior tubal ligation or removal, impaired sperm production or function, unexplained infertility, genetic disorder, or cancer treatment that preserves fertility may benefit from IVF.
Risks of IVF Cycles
IVF has relatively more risks than IUI cycles. If more than one embryo is implanted into the uterus during IVF, there is a risk of multiple pregnancies. Pregnancies with multiple fetuses are more likely to result in early labor and low birth weight than pregnancies with a single fetus. According to research, there is also a slight chance that a baby born via IVF will be premature or have a low birth weight.
When used to induce ovulation, injectable fertility drugs like human chorionic gonadotropin (HCG) can lead to ovarian hyperstimulation syndrome, which makes your ovaries painful and swollen. The typical duration of symptoms, which include mild abdominal pain, bloating, nausea, vomiting, and diarrhea, is one week. However, if you get pregnant, your symptoms might continue for a few weeks. Rarely, ovarian hyperstimulation syndrome can become more severe, which can lead to rapid weight gain and shortness of breath.
When fresh embryos are used for IVF, the rate of miscarriage is similar to that of women who conceive naturally and ranges from 15% to 25%. In contrasting cases, an ectopic pregnancy occurs when the fertilized egg implants outside the uterus, typically in a fallopian tube, and affects about 2% to 5% of women who use IVF. There is no way to carry the pregnancy on because the fertilized egg cannot survive outside the uterus.
Egg collection with an aspirating needle may result in bleeding, infection, or damage to the bowel, bladder, or blood vessels. Sedation and general anesthesia carry risks as well if used.
No matter how the child is conceived, the mother's age is the main risk factor for the development of birth defects. It is necessary to conduct more research to establish whether certain birth defects may be more likely to occur in offspring conceived through IVF.
Although some early research suggested there might be a connection between some drugs used to promote egg growth and the growth of a particular type of ovarian tumor, more recent research refutes these claims. Breast, endometrial, cervical, or ovarian cancer risk after IVF does not seem to be significantly higher.
IVF use can be physically, emotionally, and financially taxing. Therapists, family, and friends can help you and your partner get through the ups and downs of infertility treatment.
Fresh and Frozen Sperm

Fresh or frozen sperm are used in assisted reproductive technology (ART) by fertility clinics.
A sample of male sperm that is taken and used almost right away is known as fresh sperm. The fertility clinic washes the sample in a unique solution to get rid of any impurities. The sperm is then prepared for IUI (intrauterine insemination) or to create an embryo for IVF (IVF). Fresh samples are frequently utilized for couples who are working directly with a fertility clinic.
On the other hand, frozen samples are kept for future use. Using vials that are filled with a freezing solution, the samples are stored at the clinic. Liquid nitrogen is used to gradually freeze the vials after that. The process of cryopreservation keeps the sperm healthy and alive. The clinic thaws the sperm using a unique method when the sample is required.
Fresh Sperm
Fresh sperm (washed or processed sperm) are samples used at a fertility center\. They are cleaned and processed to get rid of substances that might have negative effects on the uterus. The movement (motility) and concentration of the sperm (the number of sperm per unit volume of semen) are also thoroughly checked. A concentrated amount of healthy sperm is obtained by separating the sperm from the seminal fluid, and the washed sperm is then put in a sterile liquid. Fresh samples frequently accompany egg extraction.
Couples can relax knowing that the IVF procedure uses fresh sperm samples. The clinic and the patient will be aware of the sperm's quality. Additionally, some studies show that fresh sperm-derived embryos may have a longer shelf life than frozen sperm.
Frozen Sperm
Frozen Sperm (thawed sperm) is a type of sperm that has been cleaned and prepared for freezing before being kept in a freezer for an extended period of time. When the frozen sample is ready to be used, it will be thawed until it reaches room temperature. After thawing, the sample will be examined once more to ensure that there are still healthy and viable sperm present. Sperm that has been frozen can be kept for a long time without losing viability.
Frozen sperm offers convenience. Additionally, frozen sperm is excellent for procedures such as intracytoplasmic sperm injection (ICSI).
Sperm Banking
A great way for couples (or single people) to maintain their chances of conceiving a biological child in the future is through the process of sperm banking, also known as sperm freezing or cryopreservation. This is especially true if the partner with testicles is engaged in a high-risk occupation or is about to undergo specific medical procedures or treatments.
A sperm bank or fertility center is the ideal location to store sperm for later use. After collecting a sample, sperm should be processed within one to two hours. Additionally, you can use at-home banking kits. With the help of these kits, you can gather your sperm in containers at home and send it to a laboratory for analysis and freezing. However, it’s advised by doctors to choose this option only when there are no sperm banks or fertility clinics nearby. If you choose to freeze sperm, it's crucial to consult an embryologist as they can explain the whole process and give you important reminders.
The Process of Freezing Sperm
The process of sperm banking starts by giving a sample of your blood so that you can be screened for sexually transmitted infections prior to banking your sperm (STIs).
You'll then have to complete a set of paperwork including a questionnaire, a contract, and legal forms. You will sign legal documents when you register to freeze your sperm that will specify what will happen to your sperm, for instance, if you fail to pay your storage fees. Additionally, you'll decide how the sample will be used (or discarded) by you or your partner, including in the event of your passing. For instance, you could enter into a contract that either expires upon your death or gives your spouse the authority to use it or terminate it. A notary public or a witness may be required by some clinics before you sign any paperwork.
You can provide your sample in a private area of the sperm bank or fertility clinic. As this will ensure that the sperm can be frozen at a relatively fresh state. The quantity and activity of living sperm cells start to decline shortly after ejaculation.
The quantity, shape, and movement of the sperm in the samples are then analyzed to help determine how many more samples are required. Depending on the quality of your sperm, three to six specimens are typically obtained for each desired pregnancy.
A lab technician with expertise in cryoprotectants separates the samples into numerous vials and freezes them to preserve the sperm cells. A surgical retrieval may be necessary if there is no sperm in the sample or if you are unable to ejaculate. In this situation, sperm will be taken straight from the testis by a medical professional.
The Cost of Freezing Sperm
If you freeze your sperm for a medical purpose, your insurance may occasionally cover the cost. The estimated cost is typically less than $1,000 and that includes all required testing and freezing. Costs for sperm cryopreservation range from $150 to $300 per year.
Effectiveness of Sperm Freezing
Sperm freezing is a very successful method for those who want to keep their fertility. Naturally, some sperm don't make it through the freezing procedure. The thaw survival of sperm is over 50%.
This reduction is not a problem for successfully conceiving a healthy child if the sample is of high quality. This is due to the fact that the average sperm count per milliliter of semen ranges from 15 million to more than 200 million sperm.
Nonetheless, sperm doesn't lose its potency when it freezes and thaws, and it has the same capacity for fertilization as fresh sperm. Frozen and fresh sperm also fertilize similarly.
If stored properly in liquid nitrogen and was a high-quality sample, sperm could theoretically be frozen indefinitely as well. Modern cryopreservation methods are so sophisticated that sperm integrity and health are preserved throughout the procedure.
Success Rate of Fresh vs. Frozen Sperm in Intrauterine Insemination (IUI) Cycles
In a study that looked at IUI cycles for people with ovaries who were diagnosed with unexplained infertility, researchers found that fresh sperm led to significantly higher live birth and pregnancy rates when compared to frozen sperm for IUI using ovulation-inducing medications. Age and individual drug use, which are important factors in IUI success, were not taken into account in this study.
However, the majority of fertility clinics concur that IUI can be successful with either fresh or frozen sperm. The type of sperm used has no bearing on the factors that are likely to be more crucial for IUI. Age, male infertility, sperm-related factors like sperm health, anatomical factors, and other genetic conditions can all have a significant impact on IUI infertility rates.
Success Rate of Fresh vs. Frozen Sperm in In Vitro Fertilization
During an In Vitro Fertilization (IVF) cycle, the ovaries are stimulated with fertility drugs to grow multiple follicles and mature the egg inside each follicle. The egg retrieval or egg freezing process comes next. The sperm and eggs are combined next in a lab, and then the embryos are transferred into the uterus. Ideally, the embryos implant into the uterine lining, which can lead to a pregnancy.
According to the majority of studies, using frozen sperm does not statistically significantly lower the success rate. Age, ovarian reserve, and other genetic disorders are additional variables that can have a significant impact on the success rate.
Which Type of Sperm is Best for ART Procedures?
The patient's chosen plan and whether they use sperm from a partner, a directed donor, or an unidentified donor will largely determine the sperm used in fertility treatment. Any type of sperm is acceptable, according to the majority of fertility doctors, as long as the donor's or the partner's sperm meets certain standards.
More significant than the type of sperm is the health of the patients and the sperm. IUI and IVF are both negatively impacted by the sperm of older men who have mobility and shape issues. The success of IVF cycles can be impacted by sperm quality. It's also crucial to consider a woman's overall health, including her ovarian reserve and uterine lining. It is important to take age and general fertility into account. The sperm's freshness or freezing will be the main factor in these decisions.
The aforementioned elements are far more crucial to the likelihood of conception and pregnancy than the type of sperm used in the procedure.