What are Cleavage Abnormalities?
Abnormally cleaved embryos exhibit an abnormal cleavage that includes more than two cells that resulted from a single-cell division event. At the conclusion of the division, confluent cell membranes completely separate newly formed blastomeres.
While 70% of in vitro fertilized eggs or fertilized human oocytes proceed through the initial three cleavage divisions within the first three days of culture, less than half continue on to cavitation after five days, and only around one-third develop into morphologically ideal-formed blastocysts with clearly defined inner cell mass (ICM).
Normal embryos with implantation potential may be able to develop in prolonged culture, but chromosomally abnormal embryos or aberrant and non-viable embryos may stop developing before or soon after the start of genomic activation. On the other hand, in extended cultures in preimplantation embryos in vitro, it has been demonstrated that a number of intrinsic characteristics, including sperm quality, the causes of infertility, and maternal age, affect human embryos and survival after prolonged culture.
Blastocyst formation is also connected to cleavage patterns. This feeds the connection between chromosomal defects and aberrant early human embryo development and the observed viability of in vitro developed blastocysts. However, it is obvious that the connection between embryo morphology, blastocyst morphology, chromosomal integrity, in vitro embryogenesis, and human embryo viability is more intricate. While human embryos with atypical embryo phenotypes or normal morphology can develop into blastocysts while having chromosomally defective genes or gene expression, many chromosomally normal embryos with normal cleavage and atypical or normal morphology do not differentiate in protracted culture. Additionally, some clinical evidence points to a reduction in development potential with a prolonged culture of damaged embryos. Therefore, external variables like a protracted culture period itself may also be a factor in the loss of in vitro-produced embryos or influence embryo development over time.
Barriers in Assisted Reproductive Technology
The development of various assisted reproductive technologies (ART) has significantly increased the number of live births and clinical pregnancies among patients who first report infertility. When compared to the early years of In Vitro Fertilization (IVF) and Intracytoplasmic Sperm Injection (ICSI), current live birth rates per IVF treatment cycle are significantly higher, but the reality is that overall success rates are still low, with live birth rates hovering around 21%.
Despite advancements in culture medium, laboratory tools, and techniques, only around 50% of early human embryos reach the blastocyst stage, which accounts in part for the observed poor success rates. The human preimplantation embryo's chromosomal abnormalities, human embryo ploidy, aneuploidy, or wrong chromosome copy number during the preimplantation genetic testing and early embryo viability assessment, is a crucial component in deciding the success of IVF because it can lead to implantation failure, early pregnancy loss, or chromosomally defective continued pregnancies.
Therefore, choosing the "best" euploid embryo with the greatest chance of implantation and healthy post-implantation development represents the main problem for clinical embryologists. Because there is presently no non-invasive way to view the chromosomes of the embryos, embryologists must make informed assumptions based on several scoring systems in order to determine which embryos have the most potential to successfully grow.
Identifying Cleavage Abnormalities Using Time-Lapse Imaging and Monitoring
Finding and choosing embryos with the highest developmental competence is one of the main challenges in Assisted Reproductive Technology (ART), which will ultimately improve the likelihood of conception and live birth rate. As of right now, the majority of IVF facilities around the world consider standard morphologic assessment to be the gold standard. This assessment is based on the quantity and symmetry of blastomeres, the degree of fragmentation, the presence and number of nuclei, and the size per embryo at a few static time points.
However, embryonic morphology can alter significantly during a few hours due to the dynamic nature of embryonic development. Subtle changes may therefore determine the fate of the embryos without being noticed. Time-lapse imaging is a developing solution to this problem. This is a non-invasive technology that can continually, non-invasively monitor embryos, enabling continuous embryonic monitoring, the upkeep of ideal culture conditions, and the discovery of anomalous and abnormal early cleavage events.
Introduction of Time-Lapse Monitoring to IVF
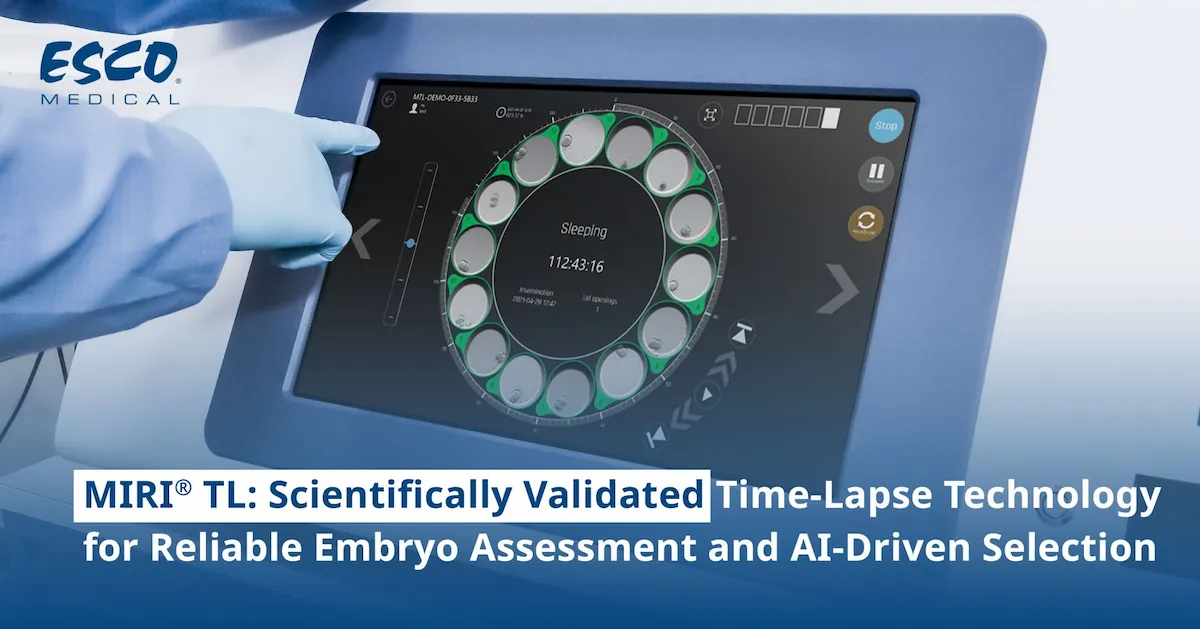
The addition of time-lapse monitoring (TLM) to IVF enables the ongoing study of early embryo development, producing more insightful data than cell counts at static time points. It not only enables the uninterrupted monitoring of the cells formed during cell cycles, four cell stages, cleavage stages, and embryonic development, but also the observation of the human cleavage stage embryos and cleavage patterns that gave rise to the daughter cells.
Through time-lapse monitoring, records of the cleavage divisions are made possible by the integration of high-resolution imaging equipment into a fully working incubator. Although there is intermittent light exposure during time-lapse imaging, this is typically less than during traditional morphological assessment. Additionally, time-lapse imaging permits transferred embryos and embryo culture in stable, uninterrupted conditions, which may be advantageous for embryo viability and the final reproductive outcome of the IVF procedure.
Morphokinetics
The majority of time-lapse studies have concentrated on morphokinetics to forecast the potential for early embryonic development. The study of morphokinetics, or the dynamics of cleavage divisions and processes like cavitation and compaction, has given biologists and clinicians a new set of information on the behavior of embryos throughout preimplantation development and its relationship to embryo quality. Numerous studies also demonstrated the value of early cleavage stage kinetics to predict normal blastocyst formation and normal development. Although choosing better-quality embryos for implantation has proven to be beneficial when using morphokinetics, this approach still offers only a limited understanding of what causes early embryonic developmental arrest.
Time-lapse imaging's added knowledge of the dynamics of embryonic divisions may aid in choosing more viable embryos for transfer, improving the embryo transfer process, and ultimately improving the reproductive outcomes (implantation and pregnancy rates) compared to a selection based solely on standard morphology assessment. However, other studies have found that despite the ability of morphokinetic characteristics to forecast an embryo's capacity to develop into a blastocyst stage, neither the rate of implantation nor the likelihood of becoming pregnant can be raised by morphokinetic analysis. It follows that the effectiveness of predictive models based on morphokinetic characteristics still has a significant impact on the usefulness of time-lapse imaging.
The application of predictive algorithms based on morphokinetics and embryo-safe time-lapse imaging technology has advanced significantly during the past ten years. Numerous morphokinetic variables have been put to the test, either alone or in combination, and it has been determined which ones are closely linked to healthy embryonic growth, whether to the blastocyst stage or full term.
Developing Comprehensive and Flexible Algorithms
Embryologists are still in the early stages of our path toward developing a common, clinical morphokinetic method for embryo selection and embryo assessment. However, they have already started the process by developing algorithms that enable accurate embryo evaluation in different labs. Embryologists and researchers need to take a further step forward and concentrate efforts on developing an algorithm that would work in various clinics and would take into account variations in IVF techniques, such as hormonal stimulation procedures, fertilization methods, and culture media, through a multi-centered validation test of morphokinetic algorithms.
MIRI® Time Lapse Incubator: Time-Lapse Imaging Technology in Your Laboratory

The MIRI® Time-Lapse Incubator by Esco Medical is a multiroom incubator with a built-in camera and microscope that can continuously capture time-lapse images of your embryo as it develops. This empowers the users with the ability to make better-informed decisions in regard to the outcome of the embryos.
It is a continuous and dynamic human embryo monitoring device that takes numerous, precise images without compromising the conditions of the embryo culture. Without needing to take the embryos from the security of the incubation chamber for manual microscopy, the MIRI® Time-Lapse Incubator offers high-quality time-lapse photographs of developing embryos in real time. Detailed morphokinetic information about the developmental stages of the embryo is available only by time-lapse monitoring, not through standard spot microscopic analysis. With the objective of increasing conception rates, this enables all significant events to be watched and assists in identifying healthy embryos with the highest likelihood of implantation.
Only the best embryos may be chosen utilizing the viewer station's embryo evaluation capabilities, which enables the early elimination of non-viable embryos. Analysis of retrospective data offers thorough documentation of patient information, medical history, and embryo data. This may also be employed for research, knowledge exchange, and embryologists' training. A measurement of the embryo can now be readily created, updated, and deleted by the embryologist. The Time-Lapse surveillance session runs up to 199 hours.
Surveillance of all embryos includes:
- The actual timing of cleavages compared to the ideal time
- The actual timing of morula and blastocyst stages
- Detecting cleavage abnormalities or abnormal cleavage embryo patterns such as Direct Cleavage and Reverse Cleavage
- Synchrony of divisions
- Multinucleation
The time-lapse imaging system integrated into benchtop incubators provides:
- Uninterrupted culture condition with separate heating chambers. Temperature and pH are crucial parameters for an optimal culture condition.
- Identification of cleavage anomalies in early stages
- Multiple, detailed time-lapse images of embryos
- Data for precise timing of a specific event through annotation procedures.
- Improvement of documentation procedures
- Develop criteria for selection/de-selection and transferring the most viable embryo(s)
Morphokinetics parameters are also important information for embryologists to decide the most viable embryo(s) for transfer.
Some of these include:
- PN formation. Assessment of appearance or fading of pronuclei. Time-lapse is able to improve assessment accuracy by knowing the exact timing of the events.
- Cell cleavage. Observe normal or abnormal cleavage embryo patterns or cleavage rate.
- Symmetry. Embryo symmetrical shape during embryo development.
- Fragmentation. Reabsorption of fragmentation only being discovered after time-lapse was introduced.
- Multinucleation of the embryo.
- Cell compaction rate and exact timing of events occurred.
CultureCoin®
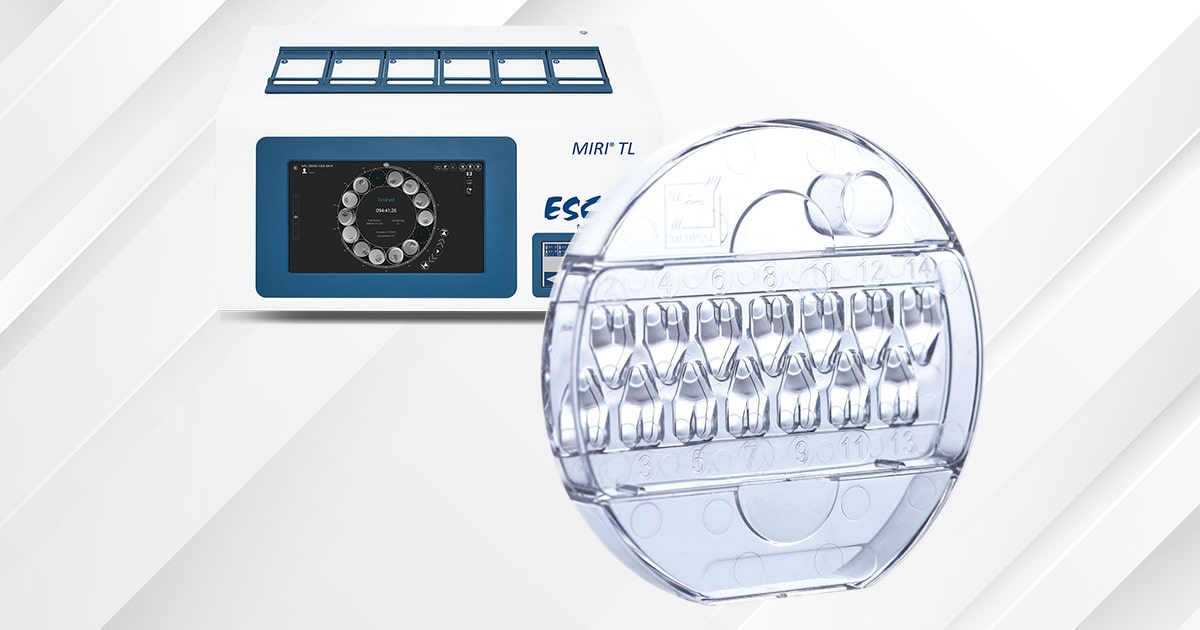
One (1) MIRI® TL chamber can hold one (1) CultureCoin®. Each dish can accommodate up to fourteen (14) embryos, each with a numbered well assignment. The MIRI® TL6 can hold up to 84 embryos, and the MIRI® TL 12 up to 168 embryos.
Key Features:
- Each embryo is cultured in its own stable environment.
- Ergonomic design for easy, safe, and secure handling of embryos.
- Independent well for pH measurements.
- Corona plasma treated surface for the effective prevention of bubble formation.
- Gamma-sterilized.