What is PICSI?
PICSI Procedure
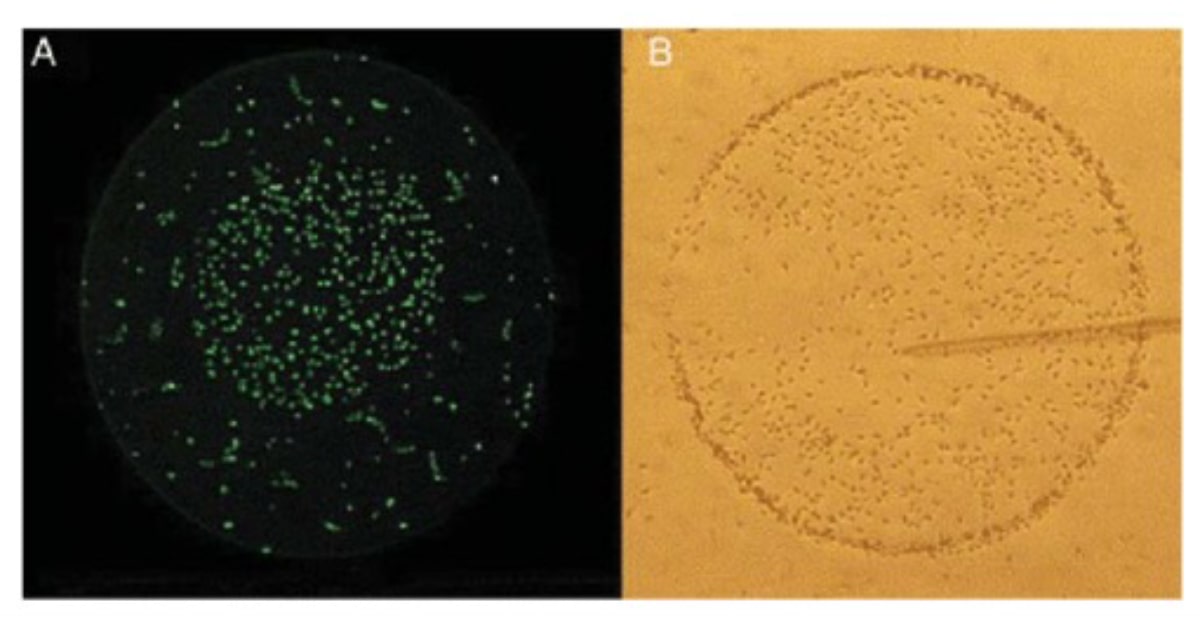
(Image 1) Sperm selection using PICSI dishes.
(A) A sperm drop is placed at the periphery of a HA drop, mature sperm binds to the HA-spot, while immature sperm moves freely.
(B) Bound sperm could be picked up with the ICSI pipette. (Jakab et al., 2005)
Advantages of using PICSI:
- Spermatozoa bound to hyaluronic acid (HA) have demonstrated lower levels of DNA fragmentation in comparison to spermatozoa prepared through density gradient centrifugation (DGC) and spermatozoa found in raw semen sample.
- The probability of enhancing a sperm population to the point where it encompasses >14% morphologically normal sperm was projected to increase 3 times after undergoing selection through HA binding.2
- Among semen samples collected from men undergoing fertility evaluations, spermatozoa bound by HA exhibited a notably reduced occurrence of autosomal disomy, diploidy, and sex chromosome disomy when compared to spermatozoa that were not subjected to HA binding selection.2
Disadvantages of using PICSI:
- It's crucial to emphasize that incorporating this additional step during the ICSI procedure will demand the embryologists to allocate extra time since the process of sperm binding alone may extend up to 30 minutes, which could present a challenge when dealing with a substantial quantity of oocytes during injection.
- The use of PICSI does not show superiority over standard ICSI in terms of enhancing the likelihood of achieving a live birth at full term, even though it does lead to a decrease in miscarriage rates.1
Who is PICSI recommended for?
- Males with high sperm DNA fragmentation.
- Patients with poor embryo quality.
- Patients with history of less or no fertilization rate.
- Patients with repeated implantation failure.
- Patients who have undergone recurrent miscarriages.
Difference between IVF, ICSI and PICSI:
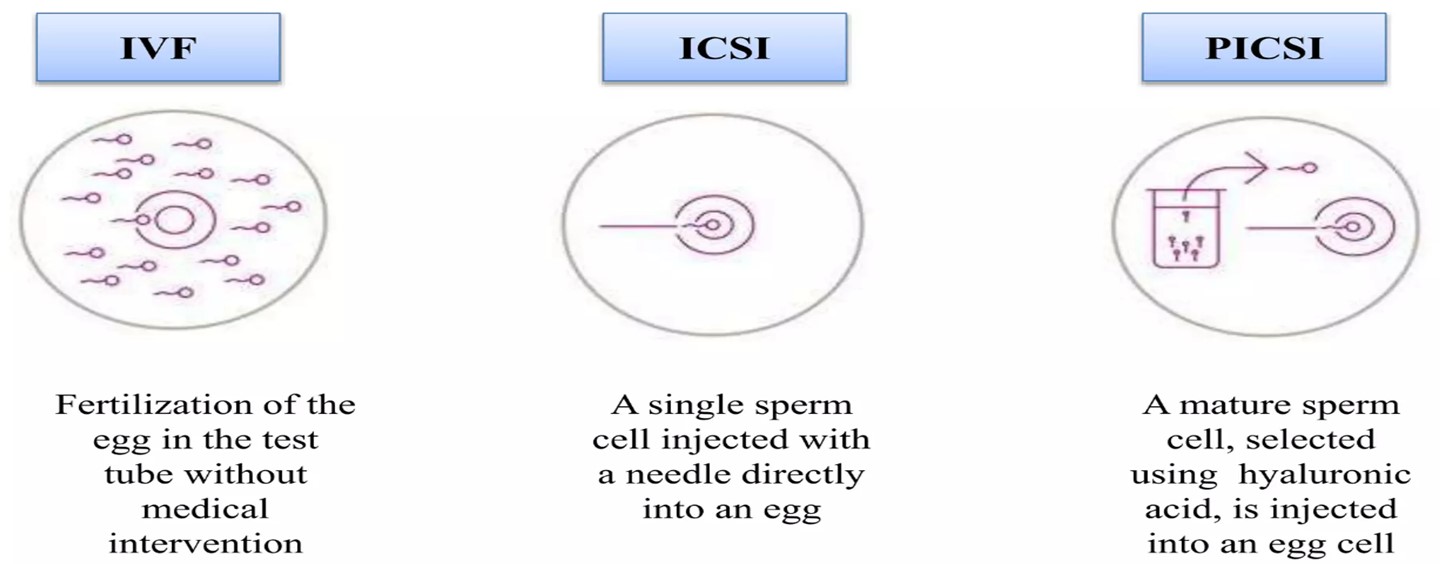
The widely employed technique in the field of ART is intracytoplasmic sperm injection (ICSI), either conventional or modified. However, in this process, the selection of sperm is based on subjective judgment by the embryologist, who chooses, based on their own criteria, the spermatozoa that appear best at low resolution. This effectively bypasses the natural selection process. Consequently, there is an increased risk of congenital abnormalities and miscarriages, as it is impossible to ascertain whether the selected spermatozoa have anomalies in their nucleus or if there is DNA fragmentation.
Hence, the physiological ICSI technique arose (PICSI - physiologically selected intracytoplasmic sperm injection).3
Research has demonstrated that by using PICSI technique, spermatozoa exhibiting binding to HA exhibit completed spermatogenic processes, including plasmatic membrane remodelling, cytoplasmic extrusion, and nuclear maturation. Consequently, they possess intact DNA with a reduced incidence of aneuploidies and miscarriages. This implies that the genomic contribution of these spermatozoa to the resulting zygotes can be likened to those selected by the cumulus oophorous during natural fertilization.
Conclusion:
The PICSI technique allows for the selection of spermatozoa based on their physiological binding capacity, enhancing the likelihood of successful fertilization and healthy embryo development. Studies have shown promising outcomes, with improved pregnancy rates and reduced risks of chromosomal abnormalities. However, it is important to note that implementing PICSI may require additional time and resources, particularly in cases involving many oocytes. Overall, the integration of PICSI into ART protocols holds great potential for further improving the success rates of fertility treatments, offering renewed hope to individuals and couples seeking to achieve their reproductive goals.
References:
1.Miller, David; Pavitt, Susan; Sharma, Vinay; Forbes, Gordon; Hooper, Richard; Bhattacharya, Siladitya; Kirkman-Brown, Jackson; Coomarasamy, Arri; Lewis, Sheena; Cutting, Rachel; Brison, Daniel; Pacey, Allan; West, Robert; Brian, Kate; Griffin, Darren; Khalaf, Yakoub (2019). Physiological, hyaluronan-selected intracytoplasmic sperm injection for infertility treatment (HABSelect): a parallel, two-group, randomised trial. The Lancet, 393(10170), 416–422.
2.Said, T. M., & Land, J. A. (2011). Effects of advanced selection methods on sperm quality and ART outcome: a systematic review. Human Reproduction Update, 17(6), 719–733.
3.Avalos-Durán, G., Ángel, A. M. E. C.-D., Rivero-Murillo, J., Zambrano-Guerrero, J. E., Carballo-Mondragón, E., & Checa-Vizcaíno, M. Á. (2018). Physiological ICSI (PICSI) vs. conventional ICSI in couples with male factor: A systematic review. JBRA Assisted Reproduction.